One of the greatest benefits of additive manufacturing (aka. 3-D printing) is the way it is making everything – from finished goods to electronic devices – cheaper and more accessible. Modern medicine is also a beneficiary of this field of technology, with new tests and possibilities being produced all the time. In recent weeks, researchers have announced ways in which it might even help lead to a cure for cancer and combat one of the greatest health epidemics of the world.
One of the greatest benefits of additive manufacturing (aka. 3-D printing) is the way it is making everything – from finished goods to electronic devices – cheaper and more accessible. Modern medicine is also a beneficiary of this field of technology, with new tests and possibilities being produced all the time. In recent weeks, researchers have announced ways in which it might even help lead to a cure for cancer and combat one of the greatest health epidemics of the world.
When it comes to testing cancer drugs, researchers rely on the traditional two-dimensional method of seeing how they work on cancer cells within the confines of a Petri dish. If the drug works well, they move onto the next stage where they see how the drug deals with 3-D tumors in animals. If that goes well, then, finally, researchers start clinical trials on humans. But if it were possible to test these drugs in a 3-D scenario right away, time and money could be saved and effective treatments made available sooner.
 And now, thanks to a team led by Dr. Wei Sun of Philadelphia’s Drexel University, this may be possible. Using the techniques of 3-D printing and biofabrication, the research team was able to manufacture tumors by squirting out a mixture of cancerous and healthy biomaterial, dollop by dollop, and create a three-dimensional replica of a living tumor. Because of this, the field of cancer research could be revolutionized.
And now, thanks to a team led by Dr. Wei Sun of Philadelphia’s Drexel University, this may be possible. Using the techniques of 3-D printing and biofabrication, the research team was able to manufacture tumors by squirting out a mixture of cancerous and healthy biomaterial, dollop by dollop, and create a three-dimensional replica of a living tumor. Because of this, the field of cancer research could be revolutionized.
According to Sun, there’s just as huge a disconnect between what works in two versus three dimensions as there is between what works in animals versus humans. These disconnects are what make developing new cancer drugs so time consuming and expensive. You can’t just rely on a formula when switching to each new environment, testing takes time, results must be documented along the way, and adjustments made at every step.
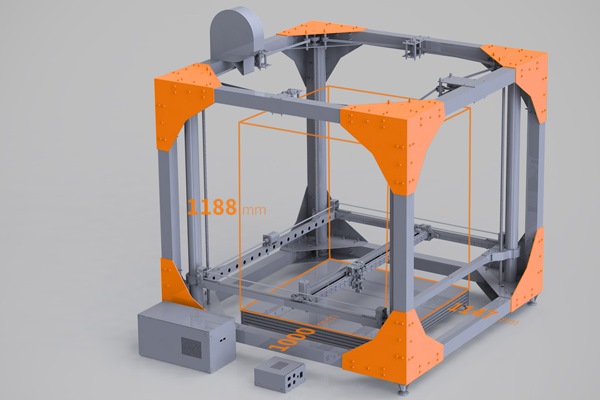
 With Sun’s 3-D printing technology, a living tumor can be printed just as easily as cancer cells grow in a Petri dish. The machinery used is capable of printing with extraordinarily high resolution, which allows cells to be placed with incredible precision. The average cell is 20 microns, where as Sun’s system can place individual cells within two to three microns. That means Sun can print out extraordinarily specific, spheroid-shaped tumors in a multitude of different shapes and sizes.
With Sun’s 3-D printing technology, a living tumor can be printed just as easily as cancer cells grow in a Petri dish. The machinery used is capable of printing with extraordinarily high resolution, which allows cells to be placed with incredible precision. The average cell is 20 microns, where as Sun’s system can place individual cells within two to three microns. That means Sun can print out extraordinarily specific, spheroid-shaped tumors in a multitude of different shapes and sizes.
But testing cancer drugs more easily is only one of the many uses of Sun’s technology. Since each tumor is different, there’s the possibility that the technology could be used to simulate individual patients’ cancers in the lab and see which drugs work most effectively on them. What’s more, Dr. Sun indicates that cancer testing is really just the beginning:
Doctors want to be able to print tissue, to make organ on the cheap. This kind of technology is what will make that happen. In 10 years, every lab and hospital will have a 3-D printing machine that can print living cells.
 On another front, 3-D printing technology is offering new possibilities in the treatment of diabetes. Often referred to as a “rich man’s disease”, this condition is actually very prevalent in the developing world where nutrition is often poor and exercise habits are not always up to snuff. To make matters worse, in these parts of the world, the disease is not considered a serious health problem and proper means and facilities are not always available.
On another front, 3-D printing technology is offering new possibilities in the treatment of diabetes. Often referred to as a “rich man’s disease”, this condition is actually very prevalent in the developing world where nutrition is often poor and exercise habits are not always up to snuff. To make matters worse, in these parts of the world, the disease is not considered a serious health problem and proper means and facilities are not always available.
Enter the Reach, a cheap new diabetes test developed by a group of students from the Schulich School of Business at York University in Toronto. Relying on 3-D printing technology, the device is aimed at urban “slum-dwellers” who may be threatened with diabetes, but very likely haven’t been checked for it. It’s one of six finalists for this year’s Hult Prize, which challenges students to create social good enterprises.
 This year’s goal, which was set by Bill Clinton, is to reduce rates of non-communicable diseases among the urban poor. As part of their Social Enterprise Challenge, the 2014 Hult Prize is intended to address the challenge of building “a social health care enterprise that serves the needs of 25 million slum dwellers suffering from chronic diseases by 2019.” And as Dhaman Rakhra, one of the students on the York research team, put it:
This year’s goal, which was set by Bill Clinton, is to reduce rates of non-communicable diseases among the urban poor. As part of their Social Enterprise Challenge, the 2014 Hult Prize is intended to address the challenge of building “a social health care enterprise that serves the needs of 25 million slum dwellers suffering from chronic diseases by 2019.” And as Dhaman Rakhra, one of the students on the York research team, put it:
We saw that diabetes is growing at the fastest rate among the slum population. It is also a disease that can be addressed, and where you can have an immediate impact. A lot of it is about a lifestyle change, if it’s detected early.
Roughly the size of a postage stamp, the Reach is similar to a home pregnancy test, in that it tests a patient’s urine. If someone’s urine has a certain level of glucose in it – indicating propensity for diabetes – the test changes color. Most importantly of all, the test can be printing out on a normal 3-D printer, making it unbelievably cheap (just two cents a pop!) The students plan to distribute the Square using the Avon business model, where local people will sell on the enterprise’s behalf.
 The Schulich students, who are all undergraduates, plan to refine the idea over the summer, first spending time with a Hult accelerator in Cambridge, Massachusetts, then during a month-long pilot test at a large slum in Mumbai. If they should win the Hult Prize, they will be awarded one million dollars to further develop, refine and finance it. But as Rakhra claimed, the real fun comes in the form of bright minds coming together to come up with solutions to modern issues:
The Schulich students, who are all undergraduates, plan to refine the idea over the summer, first spending time with a Hult accelerator in Cambridge, Massachusetts, then during a month-long pilot test at a large slum in Mumbai. If they should win the Hult Prize, they will be awarded one million dollars to further develop, refine and finance it. But as Rakhra claimed, the real fun comes in the form of bright minds coming together to come up with solutions to modern issues:
It’s exciting to really show that young people really can make a difference by creating a social enterprise that’s self-sustaining. It’s not something that many young business students really think about as a career path. But it’s definitely something we hope to influence.
The on-site manufacturing of cheap, effective drugs, prosthetics, and medical devices are undoubtedly one of the most exciting aspect of the revolution taking place with additive manufacturing. For starters, it is creating more cost effective ways to address health problems, which is a saving grace for patients and medical systems that are strapped for cash.. At the same time, it shows the potential that new technologies have to address social and economic inequality, rather than perpetuating it.
Sources: fastcodesign.com, fastcoexist.com, hultprize.org


 There is also the potential to begin reconstructive treatment with stem cells derived from adipose tissue earlier than previously possible, as it takes time for the ribs to grow enough cartilage to undergo the procedure. As Dr. Patrizia Ferretti, a researcher working on the project, said in a recent interview:
There is also the potential to begin reconstructive treatment with stem cells derived from adipose tissue earlier than previously possible, as it takes time for the ribs to grow enough cartilage to undergo the procedure. As Dr. Patrizia Ferretti, a researcher working on the project, said in a recent interview:

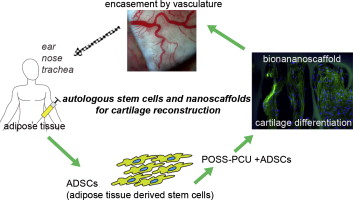





 The ability to tailor-make synthetic bones, which are exact duplicates to the original, offers exciting possibilities for reconstructive and replacement surgery. It also does away with some rather invasive and unsatisfactory procedures that involve putting shattered bones back together and joining them with pins, bars and screws. And considering that such procedures often require multiple operations, the combination of 3D scanning and 3D printed replacements is also far more cost effective.
The ability to tailor-make synthetic bones, which are exact duplicates to the original, offers exciting possibilities for reconstructive and replacement surgery. It also does away with some rather invasive and unsatisfactory procedures that involve putting shattered bones back together and joining them with pins, bars and screws. And considering that such procedures often require multiple operations, the combination of 3D scanning and 3D printed replacements is also far more cost effective.